Abstract
Background: As a source of cells for hematopoietic cell transplantation (HCT), peripheral blood stem cells (PBSC) have become a major alternative to bone marrow, the most common source of cells. A meta-analysis showed that the use of PBSC in adults is not superior with respect to overall survival, and the incidence of chronic graft-versus-host disease (GVHD) is more frequent after PBSC transplantation (PBSCT) than after bone marrow transplantation (BMT). Furthermore, several studies suggested that PBSCT in children results in poor overall survival compared with BMT, and the benefit of PBSCT is controversial. To elucidate this question, we conducted a systematic review and meta-analysis to compare the survival rate and treatment related complications of pediatric patients receiving PBSCT with those receiving BMT.
Methods: Based on the pre-defined protocol, MEDLINE, EMBASE plus EMBASE classics, Cochrane Central Register of Controlled Trials, the International Clinical Trials Registry Platform Search Portal and Clinical Trials.gov records were searched from inception through July 25, 2018 with no language restriction. The search terms included "hematopoietic stem cell transplantation" AND "allogeneic transplantation" AND "children". We included randomized control studies or cohort studies. The Newcastle-Ottawa Quality Assessment Scale was used to evaluate study quality. The primary outcome was to evaluate five-year overall survival after HCT. Secondary outcomes were five-year event-free survival after HCT, non-relapse mortality, the incidence of acute and chronic GVHD, and time to platelet and neutrophil engraftment. We performed meta-analyses using random effect models with risk ratios (RR) and a 95% confidence interval (CI). Heterogeneity was assessed using the I-squared statistic and chi-squared test. Publication bias was assessed with funnel plots.
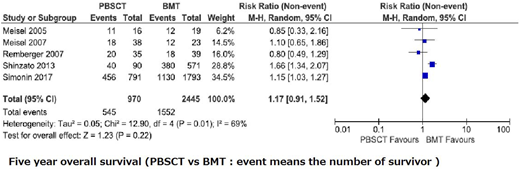
Results: We identified a total of 5,248 relevant studies. Seven cohort studies with a total of 4,328 patients (BMT group 3,185 patients and PBSCT group 1,143 patients) were included in the present study. There was no significant difference between PBSCT and BMT for five-year overall survival (RR: 1.17, 95% CI: 0.91-1.52, heterogeneity I2=69%, p=0.22) and five year event free survival (RR: 1.14, 95% CI: 0.93-1.39, heterogeneity I2=57%, p=0.05), respectively. The risk of chronic GVHD in the PBSCT group was higher than those in the BMT group (RR: 1.65, 95% CI: 1.18-2.03, heterogeneity I2=75%, p=0.002). The risk of non-relapse mortality with PBSCT was higher than with BMT (RR: 1.73, 95% CI: 1.50-1.99, heterogeneity I2=0%, p<0.00001), and the relapse rate did not show a significant difference between BMT and PBSCT (RR:1.26, 95% CI: 0.94-1.69, heterogeneity I2=71%, p=0.004).
Conclusions: This meta-analysis did not show significant difference in overall survival or relapse between PBSCT and BMT for pediatric hematological malignancy. However, a higher risk of chronic GVHD and transplantation related mortality was associated with PBSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal